Understanding the Differences Between Palliative Care and Hospice Care
Holidays are often one of the few times of the year where an entire family can get together, leave politics aside, and partake in a good meal and joyous times. However, it is often a time when a family has to make tough and difficult discussions about the health and well-being of another loved one. It is in the context that I wanted to write a article explaining both hospice and palliative care.
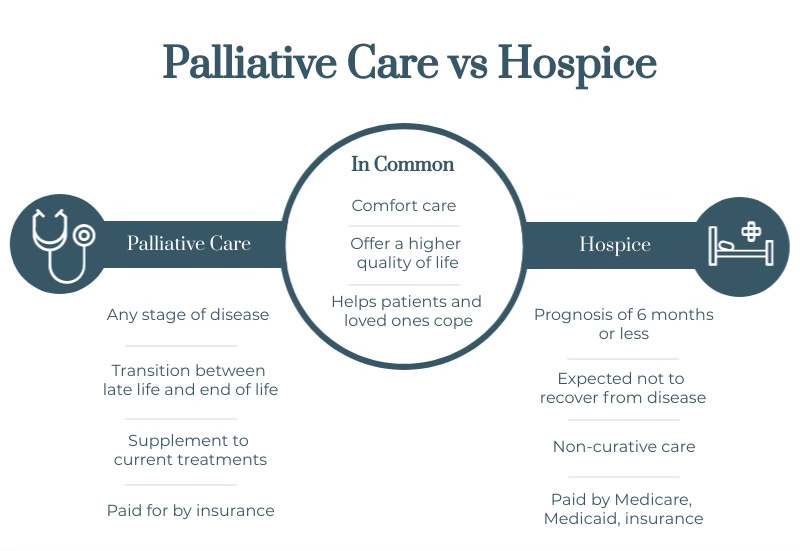
Palliative care and hospice care are often misunderstood as interchangeable terms, but they represent different philosophies and practices in the realm of healthcare focused on enhancing quality of life for patients with serious illnesses. Both approaches prioritize comfort, symptom management, and emotional support, yet they apply to distinct stages of illness and patient needs. Understanding their differences is crucial for patients, families, and healthcare providers alike.
At its core, palliative care is a specialized form of medical care designed for patients dealing with serious, chronic, or life-threatening illnesses. This approach focuses on providing relief from the symptoms, pain, and stress that accompany these conditions, irrespective of the diagnosis. The goal of palliative care is to improve the quality of life for both the patients and their families. It can be integrated at any stage of illness and is suitable for a wide range of conditions, including but not limited to cancer, heart failure, chronic respiratory diseases, kidney failure, Alzheimer’s disease, and even complex, unresolved pain syndromes. Importantly, patients do not need to be in the terminal phase of their illness to benefit from palliative care. It is often provided alongside curative treatment, ensuring that patients receive comprehensive support throughout their treatment journey.
In contrast, hospice care is a specific type of palliative care that is intended for patients who are nearing the end of life, typically with a prognosis of six months or less to live. The primary focus of hospice is on comfort and dignity during the final stages of life, rather than on curative treatment. Hospice care is generally initiated when curative measures are no longer effective or desired, allowing patients to shift their focus from aggressive treatment to quality of life enhancement, surrounded by their loved ones. Like palliative care, hospice provides a multidisciplinary team approach that includes doctors, nurses, social workers, and spiritual advisors, all working collaboratively to address the physical, emotional, and spiritual needs of patients and their families.
One of the most common misconceptions about hospice care is that it is exclusive to cancer patients. While cancer is a prevalent diagnosis among hospice patients, many others qualify for this compassionate care. Illnesses such as advanced heart disease, chronic obstructive pulmonary disease (COPD), kidney disease, neurological disorders such as amyotrophic lateral sclerosis (ALS), and even the advanced stages of dementia can lead patients to hospice care. The key criteria for eligibility in hospice is the recognition by healthcare providers that a patient is facing a terminal illness, regardless of the specific diagnosis.
Both palliative and hospice care emphasize the importance of patient choice and autonomy. In palliative care, patients are encouraged to share their goals, fears, and wishes, allowing the care team to tailor interventions that align with their values and preferences. This often includes discussions about pain management options, emotional support resources, and future healthcare decisions. Similarly, in hospice care, these values become even more critical as patients navigate the complexities of end-of-life issues. Open communication about wishes regarding life-sustaining treatments, the desire for location of care (home, hospice facility, etc.), and support for familial and spiritual needs is essential in ensuring a dignified experience.
Moreover, it’s crucial to recognize that palliative and hospice care can coexist. Patients can transition from palliative care to hospice care as their illness progresses. Alternatively, while receiving hospice care, patients may experience periods of stability that warrant a return to palliative care for symptom management, should they choose to pursue further treatment options.
In summary, while palliative and hospice care share a commitment to improving quality of life for patients with serious illnesses, they differ fundamentally in timing, goals, and eligibility criteria. Palliative care is an inclusive, adaptable approach available at any point during an illness, whereas hospice care is specifically catered to those facing imminent death. Importantly, both forms of care extend beyond cancer and encompass various serious conditions, advocating for patient dignity, comfort, and support at every stage. As awareness of these differences grows, families and patients can make informed decisions, fostering an environment where the emphasis remains on living well, even in the face of serious health challenges.
For further guidance or medical advocacy, please go to PaladinMDs because “it’s like having a doctor in the family.”


Palliative care physician here. Well said. I work on the inpatient side, and by the time I am consulted it is usually close to the end of life. So I am talking a lot about hospice since that is my recommendation at that time, adding to the confusion between palliative care and hospice. Hopefully there can be more education among medical staff to get us involved earlier in the disease process. Thanks for sharing this.
As a nurse I have seen healthcare organizations tell persons that they qualify for palliative care or convince relatives that palliative care is appropriate but when they sign on the dotted line all treatment is stopped, frequently the patient is not given appropriate choices regarding care. Nutrition and hydration as well as antibiotics are withheld under palliative care. Treatment of any type is withheld. You need to advise patients AND physicians of the difference. Neither one should be another word for euthanasia.